Bleeding Gums Are Not a Dental Issue. They’re a Systemic Warning.

What science has been quietly uncovering about oral bacteria, inflammation, and long-term health — and why most people completely underestimate what’s happening inside their own mouth.
Why brushing harder never solved the problem — and actually made it worse
For decades, oral health has been treated as a hygiene issue.
Bleeding gums? Brush more.
Bad breath? Stronger mouthwash.
Sensitivity? Scrub harder.
That logic feels intuitive. It’s also dangerously incomplete.
From a biological standpoint, bleeding is never a sign of “cleaning.”
It’s a sign of tissue breakdown.
If your gums bleed when brushed, it means the protective barrier has already failed. Those are open micro-wounds, not surface dirt. And every time that barrier breaks, it creates a direct gateway into the bloodstream.
This is where the problem stops being cosmetic — and starts becoming systemic.

Not all bacteria are equal — and some are built to survive your “oral care routine”
Your mouth hosts hundreds of bacterial species. Most are harmless. Some are protective.
But a specific group of anaerobic bacteria behaves very differently.
They do not float freely.
They do not wash away easily.
And they do not die when exposed to harsher chemicals.
Instead, they embed themselves inside microscopic cracks in teeth and gum tissue. From there, they form biofilms — protective structures that shield them from oxygen, antiseptics, and mechanical brushing.
The more aggressively you attack the surface, the more you destroy beneficial bacteria, dry the tissue, and force the harmful strains to adapt.
This is why so many people experience the same frustrating cycle:
• Bleeding improves briefly
• Breath improves for a day or two
• Then everything comes back — worse
That’s not failure of effort.
That’s biology doing exactly what it’s designed to do: survive.

Once bacteria cross the gum barrier, they don’t stay local
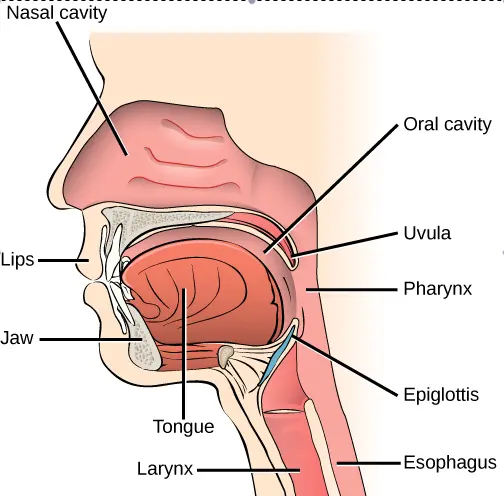
The mouth is one of the most vascularized regions of the body.
When gum tissue is compromised, bacteria don’t need to “spread.”
They simply enter circulation.
Multiple peer-reviewed studies have identified oral pathogens in:
• arterial plaque
• joint fluid
• reproductive tissue
• and brain tissue of patients with neurodegenerative conditions
This doesn’t mean oral bacteria “cause everything.”
But it does mean they are chronic inflammatory triggers — and inflammation is the common denominator in nearly every long-term disease process.
What makes this especially dangerous is that the early signals are subtle:
• mild bleeding
• persistent taste
• chronic odor
• sensitivity dismissed as “normal aging”
By the time symptoms escalate elsewhere, the original source is rarely questioned.
Healing doesn’t happen during the day — it happens when you sleep
Your body does not regenerate efficiently while under constant stimulation.
Repair happens at night.
This includes gum tissue.
This includes enamel remineralization.
This includes immune modulation.
Saliva plays a critical role here. It is not just moisture — it’s a delivery system for minerals, enzymes, and antimicrobial compounds.
But common habits — alcohol-based rinses, aggressive brushing, mouth breathing — severely suppress salivary flow for hours, especially overnight.
When saliva shuts down, the mouth becomes dry, acidic, and oxygen-deprived — the exact environment anaerobic bacteria thrive in.
That’s why mornings often feel worse than nights.
And that’s why any approach that ignores the nighttime window is fundamentally incomplete.

Because this perspective doesn’t fit traditional models
Modern dentistry is excellent at repair.
It is far less focused on biological ecosystems.
Most interventions are mechanical: drill, scrape, remove, replace.
They treat damage — not environment.
But bacterial ecosystems respond to conditions, not force.
There is growing research around enzymatic disruption of biofilms, mineral-based remineralization, and immune-supportive compounds that work with the body rather than against it.
These ideas don’t replace dentistry.
They challenge its blind spots.
And that’s why most people never hear about them until they start asking deeper questions.
If you’re the kind of person who needs to understand why something works before believing it, the next step matters.
The following presentation walks through this mechanism step by step — connecting oral biology, inflammation, and long-term health in a way most people have never seen before.
Ignoring early signals doesn’t make them disappear
Most people don’t lose health suddenly.
They lose it gradually, while dismissing early warnings.
Bleeding becomes “normal.”
Odor becomes “manageable.”
Sensitivity becomes “age.”
Until one day, the body collects the debt.
You don’t need to panic.
But you do need to understand what’s happening — before biology forces the issue.
If this page resonated, the presentation will make far more sense now.
